While patients are consumers of healthcare services, they can’t be considered customers in the traditional sense. The same is true of students. Over many years of teaching, I’ve noticed this parallel between the healthcare and education professions; both require significantly more “customer participation” to achieve desired outcomes than other industries do. That’s one reason it’s difficult to measure the quality of these institutions and the skills of their practitioners. That’s also why both industries focus so intently on engaging our communities; we simply can’t be successful unless we do.
“Can You Hear Me Now?”
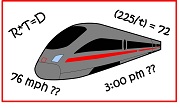
As the old joke goes, there are 3 types of people in this world: those who are good at math and those who aren’t. Many students believe themselves to be permanent denizens of the 2nd camp. They find mathematical concepts confusing and the terminology inscrutable, so they tend not to ask questions. They’re afraid they’re being judged, so they’re not always truthful. Tests and exams fill them with anxiety, and sometimes even panic (no doubt waking to nightmares of trains leaving stations at varying rates of speed). These are the students who need my help the most. Our success in overcoming these challenges together will depend heavily on the student/teacher connection we can establish, yet few students are actually able to choose the teacher with whom they are asked to connect. Sound like healthcare yet?
So it’s no surprise that trends toward greater patient engagement in healthcare, and patient-centricity in clinical research, emphasize clear and compassionate communication. Doctors, like instructors, need to explain concepts in relatable terms, encourage and address questions, assuage unwarranted anxiety, and establish trust. Until that happens, a meaningful partnership isn’t even possible.
When the Cat’s Away, Will the Mice Make Good Choices?
You may remember that old college rule of thumb: 1 hour of class requires 3 hours of study. This means instructors have just 25% of their students’ time to inspire the behaviors and habits that will make a success of the other 75%. “Don’t be the Sage on the Stage,” the mantra goes, “be the Guide on the Side.” If you’ve ever taught in an academic setting, you know how challenging that can be. The role of lecturer is fairly obvious, but the role of coach is nuanced; it evolves over time and it’s different for everyone.
And if a college instructor has just 3 hours of face time a week, a physician is lucky to have 3 hours of face time a year. That’s not much time to persuade, convince, and encourage the lifestyle choices and medication adherence essential to maintaining good health. And when you consider that a good part of each office visit is spent performing examinations and assessments, it’s easy to understand the excitement surrounding mobile health technologies. Beyond delivering real-time, real-world data, smartphone apps can send patients important reminders, make complying with diet and exercise recommendations easier, and make progress toward fitness goals visible.
“And the Survey Says…?”
Most service industries are rightly concerned with customer satisfaction – how to achieve it, how to measure it, and how to improve it. So last year, an article entitled “The Problem with Satisfied Patients” caught my eye. The Atlantic article concluded that higher hospital satisfaction ratings don’t necessarily correlate with better healthcare. A five-star student course evaluation can be similarly misleading. Pleasing a student is not the same thing as teaching a student, just as making people happy doesn’t make them well. That’s not to say that hospitals and colleges shouldn’t solicit feedback; of course they need to understand the perspective of the communities they serve. But healthcare facilities and schools should give satisfaction surveys their proper weight or they risk implementing changes that consume resources but do nothing to improve a patient’s health or increase a student’s proficiency.
Outcomes-based Evaluation
So if outcomes are paramount in both medicine and academia, it follows that the quality of care and education would be best measured by evaluating those outcomes. Right? Well, it’s a good place to start, but since patients and students share responsibility for success with their doctors and teachers, an individual outcome may be misleading. An instructor can influence, but can’t control, whether a student works on practice problems, studies for tests, asks questions, or even pays attention. A doctor can’t control whether a patient takes a prescription, follows medical advice, or reports relevant symptoms. There isn’t always a straight line between quality of service and success rate.
College instructors try to keep their students engaged by tailoring their coaching styles, offering a mix of delivery methods, seeking out fresh ideas to make the concepts relevant, and maintaining convenient office hours. Looking to improve patient engagement, healthcare systems have found that many people face situations that prevent them from keeping appointments and following medical advice. Some organizations are now providing copay assistance, arranging transportation, and employing patient care coordinators to place routine monitoring calls. None of these services are free, but they can be considerably less expensive than eating the costs associated with hospital readmissions.
The Partnership Starts Here
Teachers want their students to learn and healthcare providers want their patients to be well, but students and patients must actively participate in order to meet those goals. Handing out easy A’s and offering gourmet hospital menu items in response to survey responses won’t cut it.
Success begins with clear, compassionate communication – communication designed to explain complex concepts, to build trust, and to encourage the behaviors that lead to positive results. Understanding the challenges students and patients face enables educators and medical professionals to offer practical, meaningful solutions that can actually improve outcomes.
[In case you missed it, our last blog post was about the most common site inspection finding every year for the last decade: Protocol Deviations and How to Avoid Them.]


No comments:
Post a Comment